What Is PCOS and How Can a Vegan Diet Help Combat the Condition

An estimated one in every 10 women in the UK suffers from Polycystic Ovarian Syndrome better known as PCOS. The problem — besides what can be a debilitating and potentially heartbreaking condition — is that the misunderstood syndrome isn’t actually that familiar among the wider population, better-known acronym or not.
“It is the most common endocrine disorder in women of reproductive age,” says Rohini Bajekal, a nutritionist specialising in PCOS treatment, “although the incidence is considerably higher in certain subgroups such as those with infertility issues, certain ethnic groups, or those carrying excess weight.”
Luckily there are ways to manage the symptoms that result from the condition. Here Rohini, along with Dr Nitu Bajekal, a gynaecologist with over 35 years experience in women’s health, break down everything you need to know about PCOS, from recognising the symptoms to the whole food, plant-based diet changes that can have a life-changing impact on those who suffer from it.
Please note: we wish the terms woman/women to be used inclusively for anyone who identifies as a woman or has female reproductive organs, irrespective of their sexual orientation or gender.
What Is PCOS?
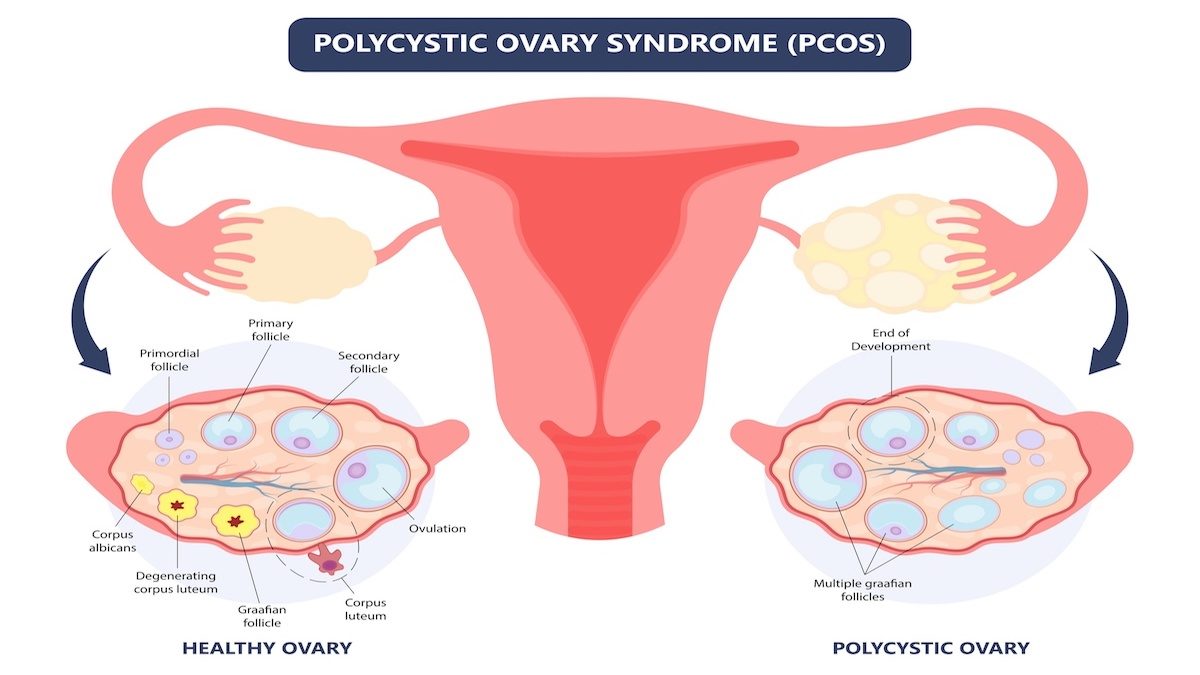
PCOS is a complex condition that affects the way the ovaries function, resulting in a wide range of reproductive, metabolic, and psychological symptoms that affect different women differently. The exact cause of PCOS is unknown, although insulin resistance, when insulin levels rise as tissues become resistant to the action of insulin, is considered to be responsible for many of the symptoms.
While PCOS is the most common cause of infertility in women, PCOS has many consequences for women that go beyond this (we’ll touch on these in the next section).
The social stigma often associated with many PCOS symptoms means women do not talk about it openly or seek the help they deserve. As many as three-quarters of those living with PCOS remaining undiagnosed. The medical definition of PCOS requires two of the three following criteria:
- Oligo, and/or anovulation (not producing eggs on a regular basis).
- Hyperandrogenism (clinical symptoms as a result of increased male hormones and/or abnormal biochemical lab tests).
- Polycystic ovaries (12 or more follicles measuring 2 –9mm in diameter and/or increased ovarian volume on pelvic ultrasound scan).
What Are The Signs You Might Have PCOS?
Symptoms of PCOS can range from weight gain to fertility problems. It is important to remember that not everyone will have all symptoms and signs of PCOS, even if they have the condition. The most common are unwanted hair growth, acne and scalp hair loss due to an excess of androgens (testosterone), and delayed or missed periods due to a lack of regular ovulation.
Most symptoms of PCOS are triggered by insulin resistance which is seen in 60-80 percent of those living with PCOS in the overweight or obese range, and in 30-50 percent of those with healthy body weight.
Increased risk of psychological and behavioural disorders, as well as reduced quality of life, have been noted in women with PCOS. A higher risk of eating disorders, and sexual and relationship dysfunction have also been seen in those with PCOS when compared to the general population. It is important to ask and screen for these psychological issues, especially depression, as per NICE guidelines.
Symptoms of PCOS:
- Infrequent periods or missed periods (Oligomenorrhoea/Amenorrhoea). Pain is not a feature of PCOS. Painful and/or heavy periods or painful sex may be signs of endometriosis, fibroids and adenomyosis, all of which can affect fertility.
- Excess facial/body hair (hirsutism).
- Acne (often adult or cystic).
- Scalp hair loss (alopecia).
- Weight gain.
- Insulin resistance.
- Fertility problems.
There are several less well-known symptoms including:
- Eating disorders. This may be missed especially in those from different ethnic groups. Referral to a dietician or another specialist (endocrinologist/dermatologist) may be indicated for some women.
- Excessive daytime sleepiness.
- Breathing problems (sleep apnoea).
- Acanthosis nigricans (darkened skin: behind the neck, underarms, groin).
- Psychological issues such as depression and anxiety which must be addressed.
- Mood disorders and sleep disturbances are now regularly associated with PCOS.
Can PCOS Just Go Away?
PCOS is a chronic condition so while there is no “cure”, making positive lifestyle changes especially through nutrition and exercise can go a very long way in managing PCOS and its symptoms, both in the short term and longer term.
Lifestyle management helps by making tissues sensitive to the action of insulin again, so insulin levels drop and as a result androgen levels drop too. Women often see their skin clearing and periods returning to normal when they make lifestyle changes.
Even where weight loss is not needed, lifestyle modifications help by improving insulin resistance. All national and international guidelines recommend lifestyle changes to be the first line of management for PCOS, even before medications. PCOS is a condition heavily influenced by our lifestyle — how we eat, sleep, move, stress, interact and so on.

Losing weight under guidance will often result in many of the symptoms getting better, especially menstrual problems. Once a diagnosis of PCOS is made, women should be counselled about the possible long-term risks. It’s important to remember that there is a lot you can do and that it’s important to seek help; genes do not need to be your destiny.
Treatment must be individualised and may be best decided with help of a specialist. Some patients may require medication such as the oral contraceptive pill or fertility treatment, alongside lifestyle changes and it’s best to weigh up all options with your health professional.
How Can A Plant-Based Diet Help?
Eating a fibre rich plant-based diet helps promote healthy gut bacteria and helps to reduce inflammation and oxidative stress, and normalises blood sugars, and lowers insulin resistance.
Given the commonality of PCOS among those with type 2 diabetes, and the higher risk of long-term consequences such as gestational diabetes, metabolic syndrome, increased cardiovascular risk factors, and womb cancer, women should be advised to focus on a predominantly whole food, plant-based way of eating.
These foods are full of fibre and micronutrients that are nourishing and absorbed slowly keeping blood sugars normal. We know this works very well in people with type 2 diabetes and metabolic syndrome.

The Food & Drink To Eat
Beans, peas, lentils, vegetables, fruits, whole grains, herbs, and spices are all great foods to eat. Aim to get your healthy fats from whole foods sources such as a handful of nuts, seeds, and avocados, and aim for two daily portions of minimally processed soy foods, like tofu, tempeh, and edamame. These soy foods are naturally rich in isoflavones, compounds that have oestrogen-like effects, as well as being rich in iron, potassium, B vitamins, and a good source of protein.
Complex starchy carbohydrates such as sweet potatoes, boiled or mashed regular potatoes with the skin are also health-promoting choices. Use salt, sugar, and small amounts of oil for flavouring purposes rather than overconsuming them, and try to make water your drink of choice.
Avoid or limit trans fats, oils, junk and ultra-processed foods, sugar-sweetened drinks, fruit juices, sugary foods such as cakes and biscuits, as these cause surges of insulin and blood sugar. They are all devoid of fibre and promote oxidative stress and inflammation. Limit barbecued and fried foods and ultra-processed foods that are high in tissue-damaging advanced glycation end products (AGEs) which are linked to PCOS, ageing, heart disease, and infertility.
A Note On Supplements
A food first approach is recommended rather than lots of unnecessary and expensive supplements, but it’s important to ensure a reliable vitamin B12 supplement on a plant-based diet. In addition, vitamin D deficiency is common in women with PCOS, and there is some evidence that vitamin D supplementation after an initial blood test to measure levels may improve reproductive function and insulin sensitivity. Other supplements that may be helpful in some cases include inositol, chromium and algae derived Omega 3s.
Other Lifestyle Changes…
It’s important to educate and empower yourself with reliable and accurate knowledge about PCOS. Learn how lifestyle interventions and conventional medicines can complement each other and be wary of self-styled experts without a clinical background or medical expertise.
As mentioned, nutrition is the cornerstone of PCOS prevention, management and lifestyle, but there are a number of other lifestyle pillars that play a crucial role too. These include:
Exercise: Regular movement in a form that you enjoy is key. Aerobic exercise and resistance training including high intensity interval training are all recommended to help improve insulin sensitivity in women with PCOS. Aim for 300 minutes of exercise per week (approximately one hour a day) and try and exercise outdoors in natural light.
Sleep and mood: Ensure a regular sleep routine with seven to nine hours of restorative sleep.
Stress management: Consider exercise, meditation, mindfulness, community work, psychotherapy or yoga to help manage stress and lower cortisol levels which makes insulin resistance worse.
You can follow Dr Nitu on Instagram and Twitter @drnitubajekal and Rohini @rohinibajekal, or via nitubajekal.com and rohinibajekal.com


















